Medical Marijuana for Epilepsy Treatment
- Parnian

- Mar 16
- 3 min read
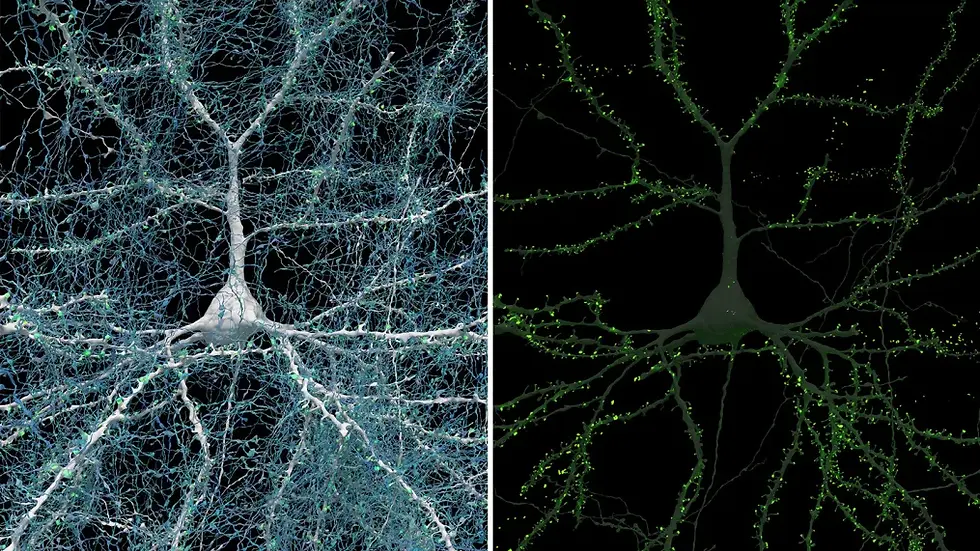
Epilepsy is a neurological disorder that affects millions of people worldwide, often causing unpredictable seizures that significantly impact daily life. Traditional treatments, such as antiepileptic drugs (AEDs), help many patients manage their condition. However, for some, these medications are ineffective or come with severe side effects. In recent years, medical marijuana has emerged as a promising alternative, offering hope to those with treatment-resistant epilepsy. This article explores the science behind cannabis-based treatments, their effectiveness, and the challenges they face in the medical community.
Understanding Epilepsy and Traditional Treatments
Epilepsy is characterised by recurrent seizures caused by abnormal electrical activity in the brain. These seizures can vary in severity and frequency, with some individuals experiencing only occasional episodes and others facing daily disruptions. Treatment typically involves AEDs, which aim to stabilise brain activity. While many patients respond well to these drugs, about 30% of individuals with epilepsy do not find relief, leading them to seek alternative therapies (Kanner).
The Role of Medical Marijuana in Epilepsy Treatment
Medical marijuana contains cannabinoids, compounds that interact with the body’s endocannabinoid system to regulate neurological functions. The two most well-known cannabinoids are tetrahydrocannabinol (THC) and cannabidiol (CBD). Unlike THC, which has psychoactive effects, CBD is non-intoxicating and has been the focus of most epilepsy research.
One of the most significant breakthroughs in cannabis-based epilepsy treatment came with the development of Epidiolex, a CBD-based medication approved by the U.S. Food and Drug Administration (FDA) in 2018. Epidiolex has been shown to reduce seizure frequency in patients with rare, severe forms of epilepsy, such as Dravet syndrome and Lennox-Gastaut syndrome (Devinsky et al.).
Scientific Evidence and Clinical Trials
Several clinical trials have supported the efficacy of CBD in treating epilepsy. A landmark study published in The New England Journal of Medicine found that children with Dravet syndrome who received CBD experienced a 39% reduction in seizure frequency compared to a 13% reduction in the placebo group (Devinsky et al.). Another study indicated that CBD treatment led to a significant decrease in drop seizures for those with Lennox-Gastaut syndrome (Thiele et al.).
Despite these promising results, medical marijuana is not a cure for epilepsy. While CBD has demonstrated effectiveness, its impact varies from patient to patient. Additionally, some individuals experience side effects such as fatigue, diarrhoea, and changes in appetite (Rosenberg et al.). More research is needed to fully understand the long-term effects and optimal dosages for different types of epilepsy.
Legal and Accessibility Challenges
The legal status of medical marijuana varies widely across the globe. In countries like Canada and parts of Europe, medical cannabis is legally accessible with a prescription. However, in many regions, restrictive laws make it difficult for epilepsy patients to obtain CBD-based treatments. In the United States, for instance, federal law still classifies cannabis as a Schedule I substance, complicating research and access despite the FDA’s approval of Epidiolex (National Academies of Sciences, Engineering, and Medicine).
Insurance coverage also poses a challenge. Epidiolex, while effective, is expensive, and many insurance companies hesitate to cover cannabis-based treatments due to regulatory uncertainties. As a result, some patients turn to unregulated CBD products, which may vary in quality and potency.
The Future of Cannabis-Based Epilepsy Treatments
The growing body of research on medical marijuana for epilepsy is encouraging, but there is still much to learn. Scientists are investigating the potential of other cannabinoids, such as cannabidivarin (CBDV), which may offer additional therapeutic benefits (Hill et al.). Future studies will help refine dosage guidelines and explore new cannabis-based formulations that could improve seizure management.
As public perception shifts and legislation evolves, access to medical cannabis may become easier for epilepsy patients worldwide. Until then, those interested in exploring CBD as a treatment should consult healthcare professionals to ensure they are using safe and effective products.
Conclusion
Medical marijuana represents a groundbreaking option for epilepsy patients, particularly those with drug-resistant forms of the condition. While research has confirmed CBD’s potential in reducing seizures, legal, financial, and medical challenges remain. With continued scientific exploration and policy changes, cannabis-based epilepsy treatments could become a mainstream option for those in need.
Sources:
Devinsky, Orrin, et al. “Trial of Cannabidiol for Drug-Resistant Seizures in the Dravet Syndrome.” The New England Journal of Medicine, vol. 376, no. 21, 2017, pp. 2011-2020.
Hill, A. J., et al. “Cannabidivarin Is Anticonvulsant in Mouse and Rat.” British Journal of Pharmacology, vol. 172, no. 10, 2015, pp. 2661-2672.
Kanner, Andres M. “Management of Drug-Resistant Epilepsy: Challenges and Strategies.” Epilepsy & Behavior, vol. 56, 2016, pp. 32-40.
National Academies of Sciences, Engineering, and Medicine. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. National Academies Press, 2017.
Rosenberg, Evan C., et al. “Cannabinoids and Epilepsy.” Neurotherapeutics, vol. 12, no. 4, 2015, pp. 747-768.
Thiele, Elizabeth A., et al. “Cannabidiol in Patients with Lennox–Gastaut Syndrome: A Randomised, Double-Blind, Placebo-Controlled Trial.” The Lancet, vol. 391, no. 10125, 2018, pp. 1085-1096.


Comments